Conversation 58: The secret of combining "the treatment focused on the reference groups [RGFT]" on the one hand, with other psychotherapeutic therapeutic approaches on the other hand
This time we will mainly discuss the possibility of combining RGFT treatment with other psychotherapeutic treatments.
We will first note that so far most of the literature articles discussing combinations of treatments in the context of psychiatric and psychological conditions refer mainly to combining a given psychotherapeutic approach with drug treatment, but as mentioned above this is not our main intention here.
In order to jump into the water, we will first start with the article by Christina Zarbo and her collegues discussing the combination of different psychotherapeutic methods.

Department of Human and Social Sciences, University of Bergamo, Bergamo, Italy
Zarbo C, Tasca GA, Cattafi F and Compare A (2016) Integrative Psychotherapy Works.Front. Psychol.6:2021.
The article by these four authors discusses the effectiveness of integrative psychotherapy, which is actually psychotherapy that combines treatments or elements from psychotherapeutic treatments and sometimes also pharmacotherapy or drug therapy. The article emphasizes the recognition of integrative psychotherapy as a valuable treatment in various psychiatric conditions while emphasizing the complexity of choosing the right psychotherapeutic approach due to the huge number of over 400 different psychotherapeutic methods are available, each defined by different theoretical models and different formats.
The purpose of the authors is to foster a dialogue between these diverse models in order to improve clinical practice.

AI-assisted illustration: the combination of several elements
The main benefits of integrative psychotherapy mentioned in the article include:
Flexibility and individualization: integrative psychotherapy allows therapists to adapt their approach to the unique characteristics and needs of each patient. This adaptability is essential for treating the diverse problems presented by different patients.
Focusing on common factors: the model emphasizes the importance of common factors that contribute to positive therapeutic results, such as the therapeutic alliance, the therapist's empathy and the client's expectations. These factors have been shown to be responsible for a significant part of the variation in the results of psychotherapy.
Comprehensive approach: Integrative psychotherapy considers different levels of functioning, including emotional, behavioral, cognitive and physiological aspects, as well as spiritual beliefs. This holistic view helps in dealing with the multifaceted nature of psychological issues.
Active participation of the client: clients are seen as active participants in their treatment, which encourages engagement and motivation. The therapist adjusts his methods according to the characteristics and preferences of the patient, and fosters a cooperative therapeutic relationship.
Evidence-based practice: The approach is consistent with the American Psychological Association's guidelines for evidence-based practice, which emphasize the integration of research evidence, clinical judgment, and client factors.
Overall, integrative psychotherapy is positioned as a responsive and effective method that can satisfy the diverse needs of patients, improve the therapeutic process and its results.
The authors propose to bridge the gap between different models of psychotherapy using the following approaches:
Promoting dialogue between models: The integrative psychotherapy movement aims to foster communication and cooperation between different psychotherapy approaches. This involves recognizing the value of different models and encouraging a framework for dialogue instead of rigid adherence to one approach.
The Common Factors Approach: By focusing on common factors that contribute to successful therapeutic outcomes – such as the therapeutic alliance, empathy and client expectations – the authors support a shared understanding that transcends specific techniques or theoretical orientations. This approach emphasizes the effectiveness of common practices in various treatments.
Research and Evidence Integration: The authors emphasize the importance of linking effective practices with their theoretical and empirical foundations. This means that integrative psychotherapy should not only apply techniques from different models, but also understand the underlying theories and research that support these practices.
Joint efforts: The article mentions the potential for collaboration between integrists [adherents of integrative psychotherapy] and psychotherapy researchers to develop a unified body of knowledge. This collaboration can lead to progress in the field of integrative psychotherapy and help clarify theoretical distinctions while maintaining the unique identities of different approaches.
Encouraging flexibility: The integrative perspective promotes a flexible and inclusive approach to different psychotherapeutic models, and allows therapists to learn from different perspectives and combine effective elements from multiple approaches as needed.
By implementing these strategies, the authors believe that the field of psychotherapy can evolve toward a more integrative and effective practice that benefits both therapists and patients.
As a rule, clinicians face several challenges in choosing a psychotherapeutic approach for patients, as emphasized in the article:
Variety of approaches: There are over 400 different types of psychotherapy, each defined by different theoretical models (eg, behavioral, cognitive, psychodynamic) and formats (eg, individual, group, family). This vast array makes it difficult for doctors to determine which approach is most effective for a specific patient or condition.
The complexity of the patient's needs: each patient presents unique characteristics, problems and contexts that require an adapted therapeutic approach. The challenge lies in the effective assessment of these personal needs and their adaptation to the appropriate psychotherapy model.
Limited dialogue between models: Historically, communication and understanding between different models of psychotherapy has been limited, which can hinder clinicians from combining techniques or insights from different approaches. This division can limit the therapist's ability to provide a comprehensive treatment plan.
Balance theory and practice: clinicians must navigate the relationship between theoretical foundations and practical application. They need to ensure that the techniques they choose are not only effective but also anchored in solid theoretical and empirical evidence.
Client factors: Clinicians must take into account client factors such as motivation, preferences and expectations, which can significantly affect the effectiveness of treatment. Balancing these factors with the chosen therapeutic approach can be challenging.
Evolving Research Landscape: The field of psychotherapy is constantly evolving, with new research findings emerging regularly. Physicians must stay abreast of these developments to make informed decisions about the most effective approaches for their patients.
Overall, these challenges highlight the need for a flexible and integrative approach that allows clinicians to tailor their practices based on the specific needs of their clients while remaining informed about the various treatment options available.
To summarize, the article describes several rules and approaches for an effective combination of different psychotherapies. Here are the key rules for combining different models of psychotherapy:
Theoretical integration: to develop a coherent framework that transcends individual models by creating a new and unified approach that integrates elements from multiple theories.
Technical eclecticism: using effective techniques from different therapeutic approaches according to their suitability to the specific needs of the client, without necessarily adhering to the theoretical foundations of these techniques.
Assimilative integration: working primarily within one theoretical model while selectively incorporating other approach techniques as needed to improve treatment effectiveness.
The common factors approach: focusing on the common factors that contribute to successful therapeutic results in different models, such as the therapeutic alliance, empathy and client expectations.
Client-centered adaptation: adapting the combination of techniques and theories to the characteristics, preferences and personal contexts of each patient, so that the treatment responds to their unique needs.
Evidence-based practices: base the combination of different treatments on empirical research and evidence, in order to ensure that the techniques and approaches chosen have proven effective.
Flexibility and responsiveness: a flexible approach to treatment must be maintained, allowing for adjustments in techniques and approaches based on the client's progress and feedback.
Collaboration between therapists: dialogue and collaboration between therapists from different directions should be encouraged in order to share insights and techniques that can improve integrative practices.
Continuous learning: one must engage in continuous professional development and training in order to stay updated about different therapeutic models and their effective combination.
Ethical considerations: Make sure that the combination of different treatments complies with ethical guidelines and proper standards, while prioritizing the client's well-being.
By following these rules, therapists can effectively combine different psychotherapeutic approaches to create a more comprehensive and personalized treatment plan for their clients.
We will now distinguish between two types of approaches: one is a combination and the other is an augmentation where the first type combines the treatments or the treatment elements from the beginning while the second combines them one after the other as reinforcement for the previous stage [where at the end of each treatment stage with a certain therapeutic approach [the benefit still does not provide enough or is only partial]. And of course it is possible to combine these two approaches when starting treatment with a combination of two methods and if there is no sufficient benefit, another therapeutic approach is added.
By the way, these concepts are taken from the world of drug treatment [mainly for depression] where augmentation is with a substance or drug that is not a classic drug for depression as opposed to a combination that combines two classic drugs for depression and where the timeline of the combination is less important.
We chose here to emphasize the difference between the two types of integration along the timeline.
We will now move on and discuss Reference Group Focused Therapy (RGFT).
It is a psychotherapeutic technique that emphasizes understanding and addressing the influence of internalized reference groups on people's psychological state. These reference groups usually consist of significant figures from the person's past, such as family members, teachers or friends, whose attitudes, behavior and expectations have been internalized and continue to unconsciously influence the person's feelings, thoughts and behavior.
Unlike the majority of therapeutic approaches that may focus on a unified "self" (such as Gestalt therapy), RGFT operates on the idea that people have multiple "selves," each shaped by different reference groups. These selves may represent various roles that the person has internalized from their social environment, especially those that are rooted in their early life or significant experiences they have had.
RGFT treatment often considers identifying these internalized characters and examining their impact on the person's behavior and mental state today. By bringing these influences into conscious awareness, people can begin to part with unhelpful or negative aspects of these internalized characters, allowing for more conscious and healthy choices in their thoughts and behavior.

AI-assisted illustration – the internalized characters that influence a person's behavior and mental state
Our approach is different from other approaches, such as Jungian therapy, which focuses on universal archetypes, or Gestalt therapy, which emphasizes the present moment and the integration of different parts of the self. RGFT focuses more on historical and social contexts that shape a person's identity and behavior [see previous blogs regarding the treatment of with RGFT]. Finally, RGFT therapy also assesses and attempts to address one's sensitivity channels.
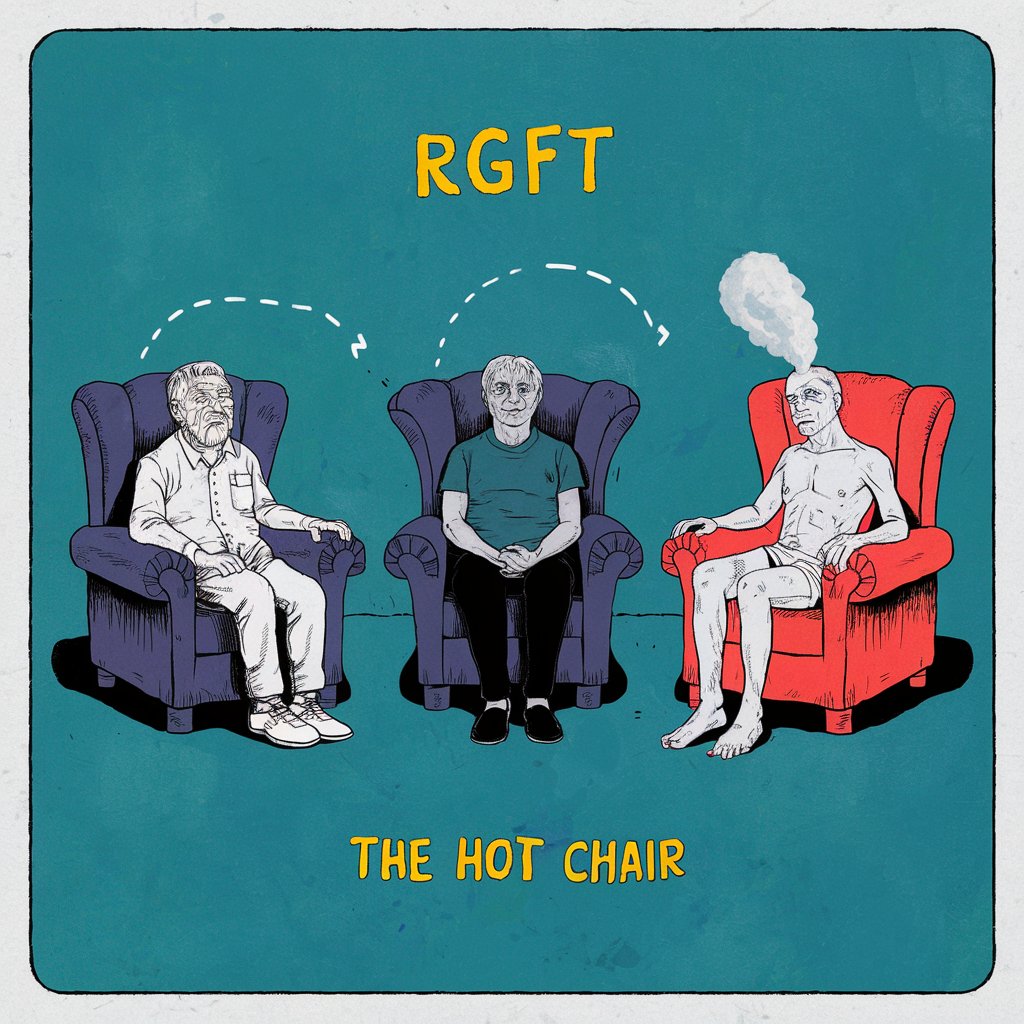
AI-assisted demonstration of a significant element in the RGFT treatment: on the left the therapist: in the middle of the patient himself: on the right the patient after moving to the hot chair and now speaking in the first person as one of the dominant internalized characters in himself.
We will now discuss the rules for combining Reference Group Focused Therapy (RGFT) on the one hand with Cognitive Behavioral Therapy (CBT) and Mindfulness Based Stress Reduction (MBSR) on the other.
Effective integration of multiple psychotherapeutic methods requires a clear set of guidelines to ensure a cohesive and beneficial therapeutic approach. Below we will offer ten rules for combining Reference Group Focused Therapy (RGFT) with Cognitive Behavioral Therapy (CBT) and Mindfulness-Based Stress Reduction (MBSR), while providing a structured framework for harmony between these therapies without conflict and maximizing therapeutic results.
Keywords: reference group focusrd therapy, cognitive behavioral therapy, mindfulness-based stress reduction, integrative psychotherapy, treatment integration, mental health
Ten rules for integration:
Rule A: Comprehensive assessment:
A thorough evaluation should be performed that includes evaluations from the perspectives of RGFT, CBT and MBSR. This holistic assessment should identify the client's internalized data, cognitive distortions and stress reactions.
Rule B: Formulation of an integrated case:
A case combining insights from RGFT, CBT, and MBSR should include an understanding of how internalized characters and sensitivity channels (RGFT), cognitive distortions (CBT), and mindfulness/stress responses (MBSR) interact and influence the client's behavior and mental health.
Rule C: Coordinated therapeutic goals:
It must be ensured that the therapeutic goals of RGFT, CBT and MBSR are clear and mutually reinforcing. Aligning this line will assist in providing a cohesive treatment plan that addresses all aspects of the client's psychological needs.
Rule D: Structured treatment planning:
Treatment sessions that combine elements from all three treatments. Initial sessions may focus on CBT for cognitive structural change, mid-treatment sessions on RGFT to explore introverted characters and sensitivity channels, and a regular mix of MBSR practices for mindfulness and stress reduction. You can also decide to start with RGFT after thinking about what is more desirable.
Rule E: Flexibility in approach:
Therapists must be flexible and willing to switch between RGFT, CBT, and MBSR techniques based on the client's immediate needs and progress. Continuous evaluation should guide these changes, ensuring that the most effective techniques are applied at the right time.
Rule F: Clear communication with the client:
Clear communication must be maintained with the client regarding the integration process. Explain to him how each approach contributes to his treatment, make sure he understands the rationale behind the use of multiple treatments.
Rule G: Regular monitoring and feedback:
The client's progress should be regularly monitored and their feedback sought. This continuous assessment helps to identify contradictions or problems at an early stage and enables timely adjustments to the therapeutic approach.
Rule H: Dealing with internal conflicts:
Therapists must be attentive to potential conflicts between internalized figures (RGFT) and cognitive distortions (CBT). These distortions can also appear in the attitudes and thoughts of the internalized characters. Use techniques from both therapies to resolve these conflicts, such as cognitive restructuring alongside exploration and reevaluation of internalized influences.
Rule I: Possibility of consistency in mindfulness practices during treatment:
There is also a situation where there is an MBSR phase consistently throughout the treatment process to improve attention and stress management. Mindfulness practices should be used to complement both RGFT and CBT techniques, and provide a stable foundation for emotional regulation. There may be therapists who will choose to practice mindfulness in the first stage or combine it as a combination from the beginning of the treatment with RGFT or CBT.
Rule J: Continuous professional development:
Therapists should engage in ongoing professional development to remain proficient in RGFT, CBT, and MBSR. Regular training and supervision ensures that therapists are equipped with the latest skills and knowledge to effectively integrate these treatments.
Combining RGFT with CBT and MBSR offers a comprehensive approach to psychotherapy, which addresses cognitive distortions, social influences and stress responses. By adhering to these ten rules, therapists can provide cohesive and effective care, and ensure that the integrated approach benefits the patient. Future research should investigate the long-term outcomes of such integrative approaches to further validate their effectiveness.

AI-assisted illustration: the combination of RGFT, CBT, MINDFULLNESS and PHARMCOTHERAPY
In order to demonstrate what was said above, we will move to an integrative approach to the treatment of a case with a specific phobia with reference group focused therapy (RGFT), together with Trigger Event Analysis (TEA) as a part of this approach, and with cognitive behavioral therapy (CBT), attention-based stress reduction (MBSR) and pharmacotherapy.
The following is a case report illustrating the treatment of a client with a specific phobia using an integrative approach that combines Reference Group Focused Therapy (RGFT), Cognitive Behavioral Therapy (CBT), Mindfulness-Based Stress Reduction (MBSR) and psychotropic medication. The report details the assessment, plan treatment, session structure and outcomes, and demonstrates the effectiveness of this multifaceted approach.
Keywords: specific phobia, reference group focused therapy, cognitive behavioral therapy, mindfulness-based stress reduction, drug therapy, integrative psychotherapy.
Introduction:
Specific phobias are intense and irrational fears of certain objects or situations that can significantly impair daily functioning. This case report provides a detailed description of the treatment process for a client named Emily, highlighting the assessment, treatment plan, session structure, and outcomes of combining RGFT, CBT, MBSR, and pharmacotherapy.
Presentation of the case:

AI-assisted illustration: Flight phobia
Background information:
Emily is a 26-year-old woman who presented with a severe specific phobia of flying (aviophobia). This phobia developed in her early teens and gradually worsened, leading to significant avoidance behavior and impairing her ability to travel for work and leisure.
The initial assessment included a comprehensive assessment from the perspective of RGFT, CBT, MBSR and pharmacotherapy:
RGFT Assessment: Emily's "council of internalized characters" included an overprotective mother who often expressed safety concerns, a risk-averse father, and a boyfriend who had a traumatic flight experience.
This data had a significant impact on her beliefs and fears about flying. Her sensitivity channels revealed heightened sensitivity to threat and attachment.
CBT Assessment: Cognitive distortions identified included catastrophic thinking (eg, belief that flying inevitably leads to disaster), overgeneralization, and excessive safety behaviors. Emily exhibited avoidance behaviors and experienced intense anxiety when thinking about flying.
MBSR Evaluation: Emily reported high levels of anticipatory anxiety and difficulty remaining calm when confronted with flight-related triggers.
Evaluation of medication: Emily had not previously used medication for her phobia, but was open to considering medication to manage her anxiety symptoms. Her psychiatrist recommended low-dose benzodiazepines (lorazepam) to be used as needed before flights, in combination with psychotherapy.
Formulation of the case:
The formulation of the case combined insights from RGFT, CBT, MBSR and pharmacotherapy:
Emily's phobia was influenced by internalized figures (RGFT) and cognitive distortions (CBT).
Her anticipatory anxiety and difficulty staying present exacerbated her phobia (MBSR).
Medication is considered to treat acute anxiety symptoms during the initial exposure to flying.
treatment plan.
The treatment plan was designed to combine techniques from RGFT, CBT, MBSR and pharmacotherapy:
Phase 1 (RGFT Focus): Initial sessions focused on exploring and re-evaluating internalized characters and sensitivity channels (through TEA).
Phase 2 (CBT Focus): The following sessions combined exposure therapy and cognitive restructuring to address cognitive distortions and reduce avoidance behavior.
Phase 3 (MBSR Focus): At the same time, MBSR practices were introduced to improve attention and reduce stress. The techniques included mindfulness meditation, body scans and mindfulness-based exposure exercises.
Pharmacotherapy Management: Emily's psychiatrist prescribed lorazepam to be taken as needed before flights or during exposure exercises. Dosage and use were carefully monitored and adjusted based on Emily's progress and side effects.
The structure of the meetings [proposal]
Session 1-4 (focus RGFT):
Purpose: To explore and reevaluate introverted characters and their influence.
Techniques: narrative therapy, role playing and analysis of sensitivity channels.
Outcome: Emily gained insight into how her past influences shaped her current fears, leading to reduced internal conflicts and anxiety about flying.
Session 5-8 (emphasis on CBT):
Purpose: to provide symptom relief and develop coping skills.
Techniques: exposure therapy (gradual exposure to flight-related stimuli), cognitive restructuring and psychoeducation about phobias and anxiety.
Outcome: Emily reported reduced avoidance behaviors and increased ability to cope with flight-related stimuli.
Purpose: to improve mindfulness and reduce stress.
Techniques: mindfulness meditation, body scans and mindfulness-based exposure exercises.
Outcome: Emily reported increased attentive awareness, reduced stress and improved emotional regulation.
Current drug management:
Coordination with a psychiatrist: regular communication with Emily's psychiatrist to monitor the effectiveness of lorazepam and adjust the dose if necessary.
Outcome: Emily experienced a significant decrease in acute anxiety symptoms during exposure exercises, which supported her engagement in treatment.
Monitoring and feedback
Regular follow-up and feedback were essential throughout the treatment process:
Progress assessments: conducted bi-weekly using standard scales for phobia severity (fear survey schedule) and anxiety.
Client’s Feedback: Emily provided feedback on her experiences and the effectiveness of various techniques.
The adjustments were made based on these assessments and feedback, while ensuring a flexible and responsive therapeutic approach.
Results
At the end of the treatment, Emily showed significant improvement:
Reduced phobia symptoms: Significant reduction in phobia symptoms as measured by the Fear Survey Schedule.
Improved emotional regulation: improved ability to manage emotions and reduced reactivity to flight-related stressors.
Increased attention: Greater awareness of the present moment and reduced anticipatory anxiety.
Effective medication: Lorazepam at a stable dose effectively managed Emily's acute anxiety symptoms with minimal side effects.
Combining RGFT with CBT, MBSR and pharmacotherapy provided comprehensive and effective treatment for Emily's specific phobia. The integrated approach addressed cognitive distortions, social influences, stress responses and neurochemical imbalances, resulting in significant improvements in her psychological well-being. Future research and clinical practice should continue to explore and validate the benefits of such integrative approaches.
This case report provides a detailed description of Emily's treatment process, and demonstrates the practical application and effectiveness of combining RGFT, CBT, MBSR, and pharmacotherapy in the treatment of a specific phobia.
We will now share another example this time about an integrative approach to treating Obsessive Compulsive Disorder (OCD) with Reference Group Focused Therapy (RGFT), Cognitive Behavioral Therapy (CBT), Mindfulness Based Stress Reduction (MBSR) and Pharmacotherapy.
The case report below illustrates the treatment of a client with obsessive-compulsive disorder (OCD) using an integrative approach that combines reference group focused therapy (RGFT), cognitive behavioral therapy (CBT), mindfulness-based stress reduction (MBSR), and medication. It details the assessment, treatment plan, session structure, and outcomes, and demonstrates the effectiveness of this multifaceted approach.
Keywords: obsessive-compulsive disorder, focus group treatment, cognitive behavioral therapy, mindfulness-based stress reduction, drug treatment, integrative psychotherapy.
Obsessive-compulsive disorder (OCD) is a complex and chronic condition that often requires a multimodal therapeutic approach. This case report provides a detailed description of the treatment process for a client named Jacob, highlighting the assessment, treatment plan, session structure, and outcomes of combining RGFT, CBT, MBSR, and pharmacotherapy.
Presentation of the case
Background:
Jacob is a 28-year-old man who presented with severe OCD characterized by intrusive thoughts related to catastrophic aspects of viral and bacterial infections and compulsive behaviors. He reported a history of anxiety and occasional depressive episodes. Jacob had previously received limited benefit from CBT alone and sought a more comprehensive therapeutic approach.

AI-assisted illustration – severe obsessive-compulsive disorder characterized by intrusive thoughts related to catastrophic aspects of viral and bacterial infections
Initial assessment
The initial assessment included a comprehensive assessment from the perspective of RGFT, CBT, MBSR and pharmacotherapy:
RGFT Assessment: Jacob's "Directorate of Internalized Characters" included a perfectionist father, a highly critical teacher, and an influential group of peers from high school and the military. These persons significantly influenced his self-perception and his compulsive behaviors. His sensitivity channels (analyzed through TEA) revealed heightened sensitivity to norms, attachment, and threat.
CBT Assessment: Cognitive distortions identified included perfectionism, catastrophic thinking and inflated sense of responsibility attitudes that could also be found in his father. Jacob exhibited compulsive behaviors such as repeated washing of his palms and body. Repeated inspection and cleaning.
MBSR evaluation: John reported high levels of stress and difficulty staying present. He often pondered his intrusive thoughts.
Medication Evaluation: John was prescribed a selective serotonin reuptake inhibitor (SSRI), specifically fluoxetine (Prozac), at a dose of 20-40 mg per day. He started the medication one month before the initial psychotherapy session.
The formulation of the case combined insights from RGFT, CBT, MBSR and pharmacotherapy:
John's OCD symptoms were related to internalized critical figures (RGFT) and cognitive distortions (CBT).
His stress response and difficulty with moment awareness contributed to his compulsive behaviors (MBSR).
Medication was necessary to manage the neurochemical aspect of his OCD, and to provide symptom relief to support psychotherapeutic interventions.
Treatment plan
The treatment plan was designed to combine techniques from RGFT, CBT, MBSR and pharmacotherapy:
Phase I (CBT Focus): Initial sessions focused on cognitive restructuring to address cognitive distortions and provide symptom relief. The techniques included exposure and response prevention (ERP) and cognitive restructuring which by the way gave a certain response to the residual sensitivity in the sensitivity channels of threat and routine [see RGFT].
Phase II (RGFT Focus): The mid-treatment sessions introduced RGFT techniques to explore and re-evaluate internalized figures and sensitivity channels. The techniques included role-playing and narrative therapy to understand the influence of internalized characters and create necessary changes and increase awareness of the influence of the sensitivity channels of the routine and the threat.
We note that in Jacob's case it was decided not to start with RGFT in light of his wishes and perceptions and indeed only after changes achieved in CBT was he more open to RGFT treatment.
Parallel phase to A and B (MBSR focus): At the same time, MBSR C practices were combined to improve attention and reduce stress. The techniques included mindfulness meditation, body scans and mindfulness-based cognitive therapy (MBCT) exercises.
Management of pharmacotherapy: Continuous coordination was conducted with Jacob's psychiatrist to monitor and adjust the medication dosage as needed based on Jacob's progress and side effects.
The structure of the meetings
Sessions 1-4 (CBT focus):
Purpose: to provide immediate symptom relief and develop coping skills.
Techniques: exposure and response prevention (ERP), cognitive restructuring, and psychoeducation about OCD.
Outcome: Jacob reported reduced compulsive behaviors and increased confidence in managing intrusive thoughts.
Sessions 5-8 (RGFT focus):
Purpose: To explore and reevaluate introverted characters and their influence.
Techniques: role play, narrative therapy, and analysis of sensitivity channels (TEA).
Outcome: Jacob gained insights into how his past influences shaped his current behaviors, leading to a reduction in internal conflicts and compulsions.
Sessions 1-10 (MBSR focus): Sessions 9-10 included reinforcement of MBSR techniques
Purpose: to improve mindfulness and reduce stress.
Techniques: mindfulness meditation, body scans and MBCT exercises.
Outcome: Jacob reported increased attention, reduced stress and improved emotional regulation.
Ongoing medication management:
Coordination with a psychiatrist: regular communication with Jacob's psychiatrist to monitor the effectiveness of the drug [fluoxetine] and adjust the dose if necessary [the dose was gradually increased from 20 mg per day to 40 mg per day].
Outcome: Jacob experienced a significant decrease in OCD symptoms with minimal side effects, which supported his practice in psychotherapy.
Monitoring and feedback
Regular follow-up and feedback were essential throughout the treatment process:
Progress assessments: were conducted biweekly using standardized scales for OCD severity (Yale-Brown Obsessive-Compulsive Scale), anxiety and depression.
Client’s Feedback: Jacob provided feedback on his experiences and the effectiveness of various techniques.
The adjustments were made based on these assessments and feedback, while ensuring a flexible and responsive therapeutic approach.
Results:
At the end of the treatment, Jacob showed significant improvements:
Reduced OCD symptoms: Significant reduction in OCD symptoms as measured by the Yale-Brown Obsessive-Compulsive Scale.
Improving emotional regulation: improved ability to manage emotions and reduced reactivity to stressors.
Increased attention: Greater awareness of the present moment and reduced rumination.
Effective medication: A stable dose of fluoxetine effectively managed Jacob's OCD symptoms with minimal side effects.
Summary:
Combining RGFT with CBT, MBSR and pharmacotherapy provided a comprehensive and effective treatment for Jacob's OCD. The integrated approach addressed cognitive distortions, social influences, stress responses and neurochemical imbalances, resulting in a significant improvement in his psychological well-being. Future research and clinical practice should continue to explore and validate the benefits of such integrative approaches. It was therefore demonstrated how combining a combination of MBSR and drug therapy with CBT followed by RGFT as augmentation resulted in good results.
Of course, according to similar principles, other treatments can be combined with RGFT. For example, in the proposals for the treatment of antisocial personality disorder with a prominent influencing social component, we wrote in Blog 55 that:
"We note that there is evidence that dialectical behavior therapy (DBT) and mentalization-based therapy (MBT) are therapeutic approaches used to treat various personality disorders, including antisocial personality disorder (ASPD).
Dialectical Behavioral Therapy (DBT) combined with mindfulness.
Initiated by: DBT Marsha Linehan in the late 1980s.
Original purpose: Originally developed to treat borderline personality disorder (BPD).
Individual Therapy: Focuses on personal issues and application of skills.
Group skills training: teaches behavioral skills in a group setting.
Telephone Coaching: Offers support between sessions.
Caregiver Advisory Team: Provides support and guidance to caregivers.
Relevance of DBT to ASPD-:
Emotional regulation: Helps people with ASPD manage intense emotions, which can reduce impulsive and aggressive behaviors.
Distress Tolerance: Teaches skills to tolerate distressing situations without resorting to harmful behaviors.
Interpersonal Effectiveness: Improves social interactions and relationships, and addresses the interpersonal deficits seen in ASPD.
Mindfulness: encourages non-judgmental awareness of the present moment, aids in self-reflection and behavioral regulation.
Efficacy: This treatment has shown promise in reducing destructive behaviors, improving emotional regulation, and improving interpersonal functioning. Its structured approach and focus on practical skills make it applicable to ASPD, although more research is needed to establish its effectiveness specifically for ASPD.
Mentalization Based Therapy (MBT)
Developers: Peter Fonagy and Anthony Bateman in the early 2000s.
Original purpose: Developed to treat borderline personality disorder (BPD).
Mentalization: The ability to understand oneself and others in terms of mental states (thoughts, feelings, intentions).
Therapeutic Relationship: Utilizes the therapist-patient relationship to explore and improve the ability to mentalize.
Group and individual therapy: combines both formats to strengthen mentalizing skills.
Relevance of MBT to ASPD:
Enhanced Empathy: Improves the ability to understand the emotions and perspectives of others, which is often impaired in ASPD.
Impulse control: A better understanding of one's mental states can lead to improved impulse control and reduced antisocial behaviors.
Interpersonal Relationships: Helps develop healthier relationships by improving communication and emotional understanding.
Comparison and complements
DBT's focus is primarily skill-based, focusing on practical techniques to manage emotions, tolerate distress, and improve relationships.
The MBT focus emphasizes understanding the mental states of oneself and others, cultivating deeper self-awareness and empathy.
Application:
Both treatments require skilled therapists and can be delivered in individual and group formats. The choice between DBT and MBT, or a combination of both, depends on the specific needs and characteristics of the person with ASPD.
And MBT offers valuable approaches to treating antisocial personality disorder by addressing key areas such as emotional regulation, impulse control, empathy, and interpersonal relationships. Further research and clinical experience will continue to refine their application and effectiveness for .ASPD.
We suggest that the understanding of antisocial personality disorder through the model of the "board of internalized characters" especially in the psychological type of personality disorder that involves the individual's upbringing environment [and does not involve genetic characteristics] which assumes a deep influence of negative internalized characters, and especially that of the dominant role of the leader – self along with activating events that reinforce antisocial behaviors, which allows for the integration of this approach in the variety of treatments offered above in ASPD, especially DBT and MBT.
It is also recommended to consider the treatment of information arising from the analysis of trigger events for the specific patient."
yours,
Dr. Igor Salganik and Prof. Joseph Levine
 Prof. Joseph Levine, M.D. is an emeritus associate professor in the Division of Psychiatry, Faculty of Health Sciences, Ben Gurion University in Israel. Prof. Levine is a certified psychiatrist with clinical experience in controlled trials of adult psychiatric disorders and in psychotherapy. He was awarded a NRSAD independent investigator grant for the study of Creatine Monohydrate in psychiatric disorders -- mainly Schizophrenia. He resides and treats patients in Tel Aviv and all of central Israel.
Prof. Joseph Levine, M.D. is an emeritus associate professor in the Division of Psychiatry, Faculty of Health Sciences, Ben Gurion University in Israel. Prof. Levine is a certified psychiatrist with clinical experience in controlled trials of adult psychiatric disorders and in psychotherapy. He was awarded a NRSAD independent investigator grant for the study of Creatine Monohydrate in psychiatric disorders -- mainly Schizophrenia. He resides and treats patients in Tel Aviv and all of central Israel.
Leave a comment